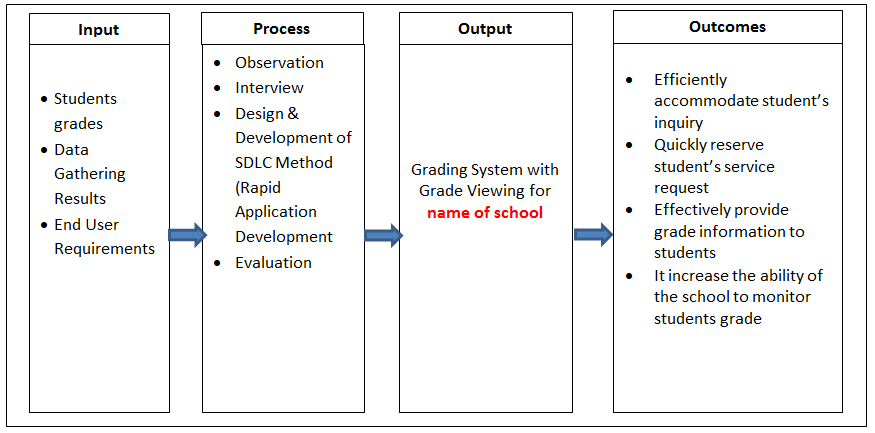
Health care benefit costs at large employers are expected to increase 6.5% in 2015, slightly lower than this year’s rate of increase. Most employers, however, say they will be able to stem increases even more as a result of changes they are making to their benefit plans, according to an annual survey by the National Business Group on Health, a non-profit association of nearly 400 large U.S. employers.
The survey also found that the number of employers offering workers a consumer-directed health plan (CDHP) as the only health benefits option is expected to surge by nearly 50% next year.
According to the survey, employers project their health care benefits costs will increase by an average of 6.5% in 2015. That is slightly lower than the 7% increase employers would have experienced this year had they made no changes to their plan design. However, employers expect to keep increases to 5% next year after making changes to their plans, such as increasing cost-sharing provisions, implementing and expanding CDHPs, and broadening their use of wellness programs and Centers of Excellence. The survey, based on responses from 136 of the nation’s largest corporations, was conducted in June 2014.
“Despite the many distractions that the Affordable Care Act (ACA) has created, large employers haven’t lost sight of the fact that rising health care costs remain a significant issue that needs to be constantly addressed,” said Brian Marcotte, president and CEO of the National Business Group on Health. “Our survey shows that many employers are, in fact, taking necessary steps to rein in costs. This includes partnering with workers to engage in health care decisions and educating them to be better health care consumers, as well as sharing more costs with workers and narrowing their benefit options.”
The survey found that employers are making numerous changes to their benefit plans in an effort to control costs as well as comply with the ACA and stay below the excise tax set to be implemented in 2018. Nearly three in four respondents (73%) are adding or expanding tools to encourage employees to be better health care consumers. More than half (57%) are implementing or expanding CDHPs while 53% will either add or expand wellness program incentives. Perhaps the most significant finding is the nearly 50% increase in the number of employers that plan to offer a CDHP as their only benefit plan option next year. Almost one-third (32%) plan to do this in 2015, compared with 22% this year.
Mixed views on private exchanges
While no employers have or intend to eliminate health benefits coverage for their active employees next year, interest in private exchanges is growing, albeit slowly. By next year, 3% of large employers will provide their active employees with health insurance through a private exchange while 35% said they are considering doing so for 2016 or beyond. Meantime, 14% of respondents are partnering with a private exchange for their retirees, an increase from 10% last year. Another 7% are planning to move retirees to private exchanges next year.
The survey, however, revealed mixed views from employers in their confidence that private exchanges will perform better than their own benefit plan. For example, 77% are confident in the exchanges’ ability to provide more choice of plans while 51% said exchanges will do a better job complying with regulations. However, only 17% are confident that exchanges do a better job of engaging employees in better health care decision making and only one in 10 believe exchanges will control costs better than their own plans.
“Employers, including many of our members, are clamoring for information and help in understanding private exchanges and whether they make sense for their organizations. The proliferation of private exchanges is presenting employers with an option but one that employers need to ask questions and study carefully. For example, employers will want to determine whether a private exchange can manage costs and care more efficiently than what they are currently doing,” said Marcotte.
Among other findings from the survey:
- Narrow Networks: Despite recent attention, only one-fourth of employers (26%) include a narrow network in any of their plans. Half of those (13%) offer a plan that incents employees to use a narrow network within the plan.
- Specialty Pharmacy Benefits: Some employers are adopting techniques specific to specialty medications to help control costs. One third (33%) use a freestanding specialty pharmacy while 29% only approve coverage for a 30-day initial supply.
- Weight Management: Nearly three-fourths of respondents (73%) will cover surgical interventions for the treatment of severe obesity while 41% will cover FDA-approved medication. Both are increases from the percent of employers that cover these this year.